The process involved in ‘making a baby’ always sounds fun and easy but for many couples this simply isn’t the case. For some the desire to conceive desperately escalates over time and month after month they find themselves far from ‘barefoot and pregnant.’ Other couples struggle with repeat miscarriages and feelings of inadequacy and disappointment. Needless to say infertility is now a global issue affecting 1 in 6 Australian couples, 1 in 5 American couples and 1 in 7 in the UK.
The process involved in ‘making a baby’ always sounds fun and easy but for many couples this simply isn’t the case. For some the desire to conceive desperately escalates over time and month after month they find themselves far from ‘barefoot and pregnant.’ Other couples struggle with repeat miscarriages and feelings of inadequacy and disappointment. Needless to say infertility is now a global issue affecting 1 in 6 Australian couples, 1 in 5 American couples and 1 in 7 in the UK.
One of the major misconceptions with regards to infertility is that couples often mistakenly believe that if they can in fact conceive but then ‘miscarry’, then the potential ‘fertility issue’ lies with the female rather than the male. Concluding that if a male can get his partner pregnant then it is not a ‘male fertility problem’. This is often not the case.
What Causes Infertility?
There are many well-documented causes of infertility including ovulatory problems such as Polycystic Ovarian Syndrome, endometriosis, uterine abnormalities, abnormal cervical mucus and sperm disorders.
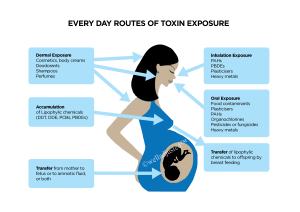
There are however also many modifiable lifestyle factors that research now demonstrates have the capacity to influence the success of fertilisation and implantation. These modifiable lifestyle factors are vastly contributing to our dramatic rise in fertility challenges. These include: macro and micronutrient status, allergies to certain foods, insulin resistance, nerve dysfunction, thyroid dysfunction, adrenal exhaustion, improper exercise and exposure to environmental toxins and chemicals.
Here are just five of the above modifiable lifestyle factors to consider:
1) Being over or under weight
Having an abnormal body mass index (BMI is the individual’s body weight divided by the square of their height) — including being underweight or overweight — can affect fertility in both males and females.
When we are underweight a hormone known as leptin is reduced. Leptin is important in regulating all functions that the body needs fat for, including ovulation. With low levels of leptin the body naturally panics and shuts down many important bodily processes and literally turns down reproduction.
When we are overweight adiponectin (a protein released by fat cells that assists in burning up fat) decreases. Adiponectin would normally help to make the body more sensitive to insulin (which enhances ovulation). Without sufficient adiponectin, over-weight people become resistant to insulin and fertility is compromised.
 2) Consider the Impact of Oxidative Stress
2) Consider the Impact of Oxidative Stress
Oxidative stress maybe the latest buzz but it’s impact is heavily linked with many chronic diseases and fertility challenges. In essence it means cell damage created by free radicals. When we are exposed to environmental stress such as pollution, radiation, toxins in the home and work place, caffeine, smoking and drug use for example, the body accumulates oxidative stress. This may result in significant damage to cell structures.
For example high oxidative stress may damage the sperm’s cell membrane and sperm DNA, leading to single or double strand breaks referred to as DNA fragmentation. If DNA fragmentation is left unrepaired it can render the sperm malformed, immobile or both. Defective sperm unfortunately can also cause miscarriage hence repeat miscarriages are not always a “female” issue.
For women, oxidative stress impairs follicles and ovaries, decreases fertilisation and the likelihood of implantation, increasing the chance of miscarriage.
3) Gender-Benders
Additionally these toxins outlines above also influence the endocrine system. Hormone disruptors or endocrine disrupting chemicals (EDCs) found in our environment are quickly becoming known as ‘gender-benders’ as they mimic oestrogen and other important chemicals that help run our bodies. Fifty one synthetic chemicals are now identified as hormone disrupters, which can disrupt the chain of hormone release needed for ovulation, fertilisation and implantation of the embryo. EDC’s are present in household cleaning products, body care products, furniture and building materials, and even in the foods we eat.
4) Nerve Dysfunction
Nerve messages can be impaired by spinal subluxations which occur when there are misalignments of the spine or pelvis. This results in altered joint motion and nerve irritation which can with time, lessen organ function and general health. In essence the body moves further and further away from homeostatic balance, which challenges the body’s central intelligence to clearly coordinate and govern functions such as reproduction.
The nerve messages that initiate and sustain reproduction (or any vital function) may in turn be compromised. It is both the severity of the subluxation and the length of time it has been left uncorrected that dictates the impact on body function.
Chiropractors adjust spinal misalignments to help restore clear function of the nervous system supporting the body to recreate ‘body order’ optimizing a couple’s likelihood of conceiving. Here we see one example of how chiropractic focuses on overall good health and function and not merely back pain and headaches.
5) Micro-Nutritional Deficiencies
While I am a big fan of sourcing nutrition through real foods there are certain times I believe we need to also address micro-deficiencies through herbs and vitamin supplements. Micro-nutritional deficiencies can result from many things including stress, smoking, other toxins, poor diet, some prescriptive medications and the contraceptive pill. Chinese Medicine practitioners and naturopaths can help ascertain and balance deficiencies you may be experiencing.
 The Good News
The Good News
While it can be extremely disheartening to experience fertility challenges an important thing to remember is that this issue can be approached as an opportunity for the couple to engage in an active plan to improve their overall health and wellbeing, rather than solely a quest to reproduce.
I am not suggesting that all fertility challenged couples are unhealthy far from it, many have worked extremely hard on living a clean, and wellness oriented lifestyle. What I am suggesting is that whether we are only just considering the impact our current health status has on our capacity to conceive or whether we are in fact a ‘long-term health guru’ there is always so much to learn about how our changing world impacts our health goals.
When we focus on our wellbeing we not only improve our capacity to naturally conceive but in doing so potentially we are more likely to have a healthy, complication-free pregnancy and a healthy child.
For more information please see Well Adjusted Babies 2nd Edition and our blog posts at https://welladjusted.co
. . . . .
Jennifer Barham-Floreani
Bach. Chiropractic, Bach. App Clinical Science
Registered internationally, no longer practicing as a chiropractor in Australia.
REFERENCES
Global infertility and the globalization of new reproductive technologies: Social Science & Medicine 2003;56: 1837–1851
National Fertility Study 2006 Australian’s Experience and Knowledge of Fertility Issues. The Fertility Society of Australia. Dr Anne Clark.
Cahill and Wardle, BMJ 2002; 325: 28 – 32
Wallace W.,Hamish B.,TW. Kelsey (2010-01-27). “Human Ovarian Reserve from Conception to the Menopause” PLoS ONE 5 (1): e8772. doi:10.1371/journal.pone.0008772.
The adverse effects of obesity on conception and implantation – Christopher J Brewer and Adam H Balan – 2010 Society for reproduction and fertility ISSN 1470-1626 (paper) 1741-7899 (online)
Homan G, et al. The impact of lifestyle factors on reproductive performance in the general population and those undergoing fertility treatment: a review. Hum Reprod Update 2007;13(3):209-233.
Y Li, H Lin, J Cao. Association between socio-psycho-behavioral factors and male semen quality: systematic review and meta-analyses Fertil Steril. 2010 Jul 30. [Epub ahead of print]
Kalantaridou SN, et al. Corticotropin-releaseing hormone, stress and human reproduction: an update. J Reprod Immunol. 2010 May;85(1):33-9
Oliva A, et al. Contribution of environmental factors to the risk of male infertility. Hum Reprod 2001;16(8):1768-1776.
Swan S, et al. Semen quality in relation to biomarkers of pesticide exposure. Environ Health Perspect 2003;111(12):1478-1484.
Abell A, et al. High sperm density among members of organic farmers’ association. Lancet 1994;343:1498.
National Children’s Study Workshop Expanding Methodologies for Capturing Day-Specific Probabilities of Conception May 17–18, 2004 Led by a consortium of federal agency partners: the U.S. Department of Health and Human Services (including the National Institute of Child Health and Human Development [NICHD] and the National Institute of Environmental Health Sciences [NIEHS], two parts of the National Institutes of Health, and the Centers for Disease Control and Prevention [CDC]) and the U.S. Environmental Protection Agency (EPA).
Sharpe RM, Irvine DS. How strong is the evidence of a link between environmental chemicals and adverse effects on human reproductive health? BMJ 2004; 328(7437):447-51
S Tas, R Lauwerys and D Lison: Occupational hazards for the male reproductive system. Critic Rev Toxicol 26, 261–307 (1996)
Oliva A, et al. Contribution of environmental factors to the risk of male infertility. Hum Reprod 2001;16(8):1768-1776.
Sharpe RM, Irvine DS. How strong is the evidence of a link between environmental chemicals and adverse effects on human reproductive health? BMJ 2004; 328(7437):447-51
Chemicals in Many Cosmetics Detrimental to Your Unborn Son. Environmental Health Perspectives May 27, 2005 Cited in https://articles.mercola.com/sites/articles/archive/2005/07/02/cosmeticchemicals.aspx [Unavailable] 10Keen C et al.The Plausibility of Micronutrient De?ciencies Being a Signi?cant Contributing Factor to the Occurrence of Pregnancy Complications. 2003 American Society for Nutritional Sciences)
L Chasan-Taber, WC Willett et al. Oral Contraceptives and Ovulatory Causes of Delayed Fertility. Am J Epid.1997.Vol 146, No 3. 12Agarwal A, Sekhon LH. The role of antioxidant therapy in the treatment of male infertility. Hum Fertil (Camb). 2010 Dec;13(4):217-2513Anderson K, et al. Lifestyle factors in people seeking infertility treatment- A review. Aust & NZ J Obstet Gynaecol.2010 Feb; 50(1);8-20. 14British Medical Association Smoking and reproductive life: The impact of smoking on sexual, reproductive and child health Feb 200415Bolumar F, et al. Caffeine intake and delayed conception: a European multicenter study on infertility and subfecundity. Am J Epidemiol 1997;145:324–334.
Fronczak CM, Kim ED, Barqawi AB. The Insults of Illicit Drug Use on Male Fertility. Published-Ahead-of-Print on July 28, 2011 by Journal of Andrology.
Bracken MB, Eskenazi B, Sachse K, McSharry JE, Hellenbrand K, Leo-Summers L. Association of cocaine use with sperm concentration, motility, and morphology. Fertil Steril. 1990;53:315-322.
Saso L. Effects of drug abuse on sexual response. Ann Ist Super Sanita. 2002;38(3):289-96.
Mueller BA, Daling JR, Weiss NS, Moore DE. Recreational drug use and the risk of primary infertility. Epidemiology. 1990 May;1(3):195-200.