What if I could share with you some of the lifestyle habits or choices we make that may impact our child’s (and our own) immune strength and digestive power — would you be intrigued?
What if I could share with you some of the lifestyle habits or choices we make that may impact our child’s (and our own) immune strength and digestive power — would you be intrigued?
Since turning my attention to the risk factors that make children susceptible to allergies, eczema, asthma and developmental delays I am constantly reminded at how the body works as a whole rather then individual parts or systems. We hear a lot about an ‘over sensitive’ immune system or a ‘weak’ digestive system or children who are ‘developmentally’ delayed and we see many varied approaches for trying to rectify these specific health issuses. More often then not however many of these approaches (even those taken by holistic practitioners) often only address one “system” of the body. They may for example only focus on restoring gut function rather then taking a multi-faceted approach to nurture and restrengthen the body as a whole.
What I want to impress upon you is the importance of the Gut-Brain-Immune Axis and how when this interconnected system is ‘derailed’ — all hell breaks loose in relation to our own health or the health of our children.
So What The Heck Is The “Gut-Brain-Immune Axis” & Why Should I Care?
Well through its interconnection the Gut Brain Immune Axis (GBI axis) controls most functions in the body, it compromises of three parts:
- the gut (encompassing the gastrointestinal tract and related detoxification organs such as the liver)
- the immune system
- the brain (including all components of the central nervous system or CNS)
All three systems form a complex, inter-related communication network that control how we perceive and respond to our environment.
It is important that we understand that there are a number of events/factors that may occur:
- during pregnancy
- during birth
- early childhood
These have now been suggested to derail this GBI axis and may increase our susceptibility to allergies, asthma, eczema, ADHD, autism, autoimmune disease and a host of other health challenges. I have briefly outlined these risk factors in a graphic later in this post.
For adults many of these factors have stirred our GBI axis for decades and unknowingly we further exacerbate the issue through choices we make on a daily basis. With time, our health becomes completely derailed and there’s no surprise that most days we feel like a ‘train wreck’ physically and emotionally. We wonder why we don’t find the same buzz from caffeine and stimulants, why we don’t feel long-lasting energy from sleep or exercise like we use to and why a course of antibiotics may seem to work initially but then sweep us further down the health scale, vulnerable to more and more infections. The human body works together as one and how we tax our body physically, chemically and mentally impacts our short and long-term health.
“But what about genes, aren’t they responsible for many of these issues?”
Some of you may be itching to now ask the role genes play in how sickness and disease manifest.
While there may be a gene component in certain scenarios for some individual cases, for most adults and children who face these health challenges genes are not the key player and most lead researchers come back to this theme, “Genetics may load the gun but the environment pulls the trigger.” This is why in many families only one sibling will develop allergies, autism or autoimmune disease and other family members do not.
Four Important Points:
- 70-80% of our immune system is found in the gut (our digestive tract).1
- Children are particularly susceptible to GBI axis dysfunction because their gut, brain and immune systems are still developing and are therefore vulnerable.2
- A child’s digestive system may be somewhat leaky and their liver detoxification systems are immature this means young children are not very capable of handling harsh metals and toxins. Young children may experience increased levels of systemic inflammation and oxidative stress in response to minimal amounts of toxins.3
- A child’s blood-brain barrier (BBB) is not fully intact until at least two years of age, leaving the CNS highly susceptible to damage.4
Factors That Drive Dysfunction Of The Gbi Axis
With this graphic I have outlined a number of potential risk factors that are now suggested to DEFAULT or negatively impact a child’s (or adults) digestive function, immune strength and overall gut, brain, immune co-ordination.5 Again many of these may arise prior to pregnancy, during pregnancy and post birth but often it is the compound (build-up) effect of these factors that results in offsetting this important connection with the systems of the body.
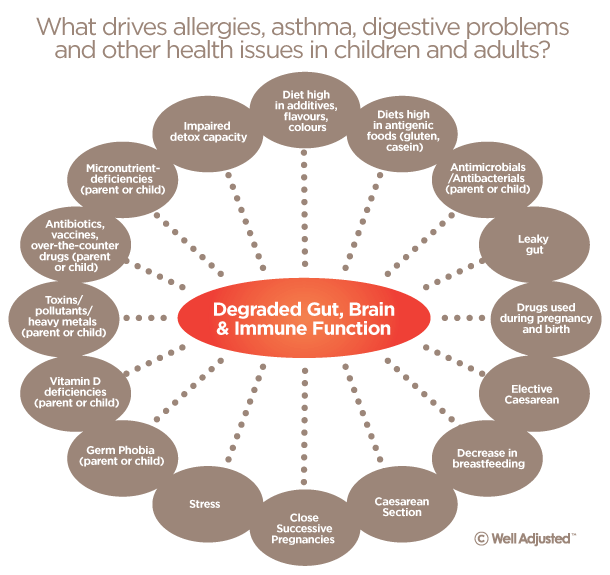
Over the counter drugs, paracetomol for example and many prescriptive drugs while at times they may be recommended, when taken during pregnancy and in early childhood particularly, deplete the body of important micro-nutrition and promote excessive inflammatory immune responses.6
In this series of posts we are going to look at how many of these lifestyle factors impact the health and strength of the gut, immune system and their connection with the nervous system. We will also look at ways we can combat choices we may have made in the past that have potentially compromised these areas of our body or our child’s health and focus on what proactive steps we can take to restrengthen and rebalance our clever bodies.
. . . . .
From the desk of…
Jennifer Barham-Floreani
Bach. Chiropractic, Bach. App Clinical Science
Registered internationally, no longer practicing as a chiropractor in Australia.
. . . . .
2 – 5)
i. Luebke RW, et al Immunolotoxicology Workgroup.The comparative immunotoxicity of five selected compounds following developmental or adult exposure. J Toxicol Environ Health B Crit Rev. 2006 Jan-Feb;9(1):1-26
ii. Grammatikos AP. The genetic and environmental basis of atopic disease. Ann Med. 2008;40(7): 482-95
iii. Macdonald TT, Monteleone G.Immunity, Inflammation, and allergy in the gut. Science 2005;307:1920-5
iv.Holladay SD, Development of the murine and human immune system: differential effects of immunotoxicants depend on the time of exposure. Environ Health Perspect. 2000 Jun;108 Suppl 3:463-73
v. Beasley R, teal. Association between paracetamol use in infancy and childhood, and risk of asthma, rhinoconjunctivits and eczema in children aged 6-7 years: analysis from Phase three of the ISAAC programme. lancet. 2008 Sep 20;373 (9643):1039-48
vi. McKeever TM et al.Am J Resp Crit Care Med 2002 vii.Schulze etal AM J Clin Nutr 2005;82:675-84
viii. Douglas AJ. Baby On Board: Do responses to stress in the maternal brain mediate adverse pregnancy outcome? Frontiers in Neuroendocrinolgy 31(2010) 359-376
ix. Prakash S teal. Gut microbiota: next frontier in understanding human health and development of biotherapeutics. Biologics. 2011; 5:71-86
x.Shaheen SO. et al Paracetamol use in Pregnancy and wheezing in early childhood. Thorax 2002:57:958-963
xi.Decker E. “Cesarean Delivery Is Associated With Celiac Disease but Not Inflammatory Bowel Disease in Children” Pediatrics 2010;125;e1433; originally published online May 17, 2010; DOI: 10.1542/peds.2009-2260
xii. Mårild OS, “Pregnancy outcome and risk of celiac disease in offspring: A nationwide case- control study”Gastroenterology. 2012 January ; 142(1): 39–45.e3.
6) i.Beasley R, teal. Association between paracetamol use in infancy and childhood, and risk of asthma, rhinoconjunctivits and eczema in children aged 6-7 years: analysis from Phase three of the ISAAC programme. lancet. 2008 Sep 20;373 (9643):1039-48
ii .Shaheen SO. et al Paracetamol use in Pregnancy and wheezing in early childhood. Thorax 2002:57:958-963


 What if I could share with you some of the lifestyle habits or choices we make that may impact our child’s (and our own) immune strength and digestive power — would you be intrigued?
What if I could share with you some of the lifestyle habits or choices we make that may impact our child’s (and our own) immune strength and digestive power — would you be intrigued?