Inflammation – heard of it? I’m sure you have as it’s one of the new buzz terms that people are now frequently talking about. The reason being is that it is widely acknowledged that inflammation drives many of our disease processes.
“What do brain fog, flat mood, depression, and constipation have in common?”
“How about heart disease, obesity, diabetes, metabolic syndrome, rheumatoid arthritis, gout, asthma, psoriasis, and other chronic conditions?”
The answer, yes – inflammation.
The right kind of inflammation is essential to your body’s healing system. But chronic inflammation can be a problem. The saying “too much of a good thing” applies to much of life, but especially to inflammation.
 So, what is inflammation?
So, what is inflammation?
Inflammation happens in everyone, whether we are aware of it or not. Inflammation is the immune system’s response to harmful stimuli (such as pathogens), from damaged cells (disease), toxic compounds, or radiation. It is how the immune system acts by removing these injurious stimuli and how it initiates the healing process.
Those traumas or harmful stimuli may come in different forms, physical (a bone fracture, cut or scrape, burn, or rash), dietary (processed food, fried food, sugar, allergenic foods), and environmental (mold, metal toxicity, chemical-laden cleaning, and personal care products).
Inflammation is therefore a defense mechanism that is vital to health.
We hear more and more about inflammation these days as it underscores not only preventable diseases but also gut dysfunction. Usually, during an acute inflammatory response, cellular and molecular events efficiently minimize impending injury or infection. This mitigation process contributes to the restoration of tissue homeostasis (balance) and the resolution of the acute inflammation. However, uncontrolled acute inflammation may become chronic, contributing to a variety of chronic inflammatory diseases1.
Many people aren’t aware of the fact that the gut is the biggest potential source of inflammation in the body. Think of chronic inflammation as a smoldering fire that takes time to put out and your poor gut health as the lighter that sparks the flames of that inflammation. What starts in the gut can eventually affect nearly every organ in your body. But, like the silent embers of a low-burning flame, inflammation is not always obvious to the person it controls.
Chronic inflammation takes up a lot of immunity bandwidth that could otherwise be better spent on our frontline of defense against viruses and pathogens. It’s imperative to get inflammation under control if you want to maximize immunity and your general health and wellbeing.
Types of Inflammation
Acute Inflammation:
Tissue damage due to trauma, microbial invasion, or toxic compounds can induce acute inflammation. It starts rapidly, becomes severe in a short time and symptoms may last for a few days, for example, a sprained ankle, cellulitis, or acute pneumonia. Subacute inflammation is the period between acute and chronic inflammation and may last 2 to 6 weeks.
 Acute inflammation produces obvious and immediate symptoms such as:
Acute inflammation produces obvious and immediate symptoms such as:
- Redness
- Pain
- Warmth
- Swelling
Chronic Inflammation:
Chronic inflammation is also referred to as slow, long-term inflammation lasting for prolonged periods of several months to years. Generally, the extent and effects of chronic inflammation vary with the cause of the injury and the ability of the body to repair and overcome the damage.
Chronic inflammation is a more gradual and subtle process. When symptoms do appear, they can include3:
- Fatigue
- Headaches
- Muscle aches, joint pain, body pain,
- Skin rashes, eczema, dermatitis, and psoriasis
- Excess mucus, Frequent colds, and flu,
- Frequent infections of other kinds like sinusitis
- Weight gain or weight loss
- Extra belly fat
- Facial swelling
- Insomnia
- Lymph nodes are swollen
- Constipation, diarrhea, and other gastrointestinal issues like constipation, diarrhea, and acid reflux
- Depression, anxiety, and mood disorders
- Chronic fatigue
Unlike with acute inflammation, these symptoms continue long-term or come and go over time.
How Does Inflammation Work?
Inflammation is the first step in the healing process. As we outlined above at the tissue level, inflammation is characterised by redness, swelling, heat, pain, and loss of tissue function, which result from local immune, vascular, and inflammatory cell responses to infection or injury1. Examples of a loss of function include not being able to move an inflamed joint properly, loss of smell during a cold or flu, or finding it more difficult to breathe when you have bronchitis.2
When cells are damaged, they send out chemical messengers that cause swelling, which isolates the offending substance and keeps it from penetrating more cells. The chemical messengers also call white blood cells to the site of injury to get rid of bacteria and dead or damaged cells. The resulting product is pus.
Click here for a more detailed explanation of which immune cells are involved and an understanding of the inflammatory steps.
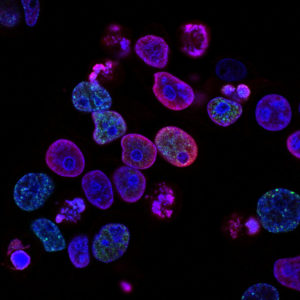
When inflammation occurs in your body, many different immune system cells may be involved.
- They release various substances, known as inflammatory mediators. These include the hormones bradykinin and histamine. They cause the small blood vessels in the tissue to become wider (dilate), allowing more blood to reach the injured tissue. For this reason, inflamed areas turn red and feels hot.2
- The increased blood flow also allows more immune system cells to be carried to the injured tissue, where they help with the healing process. What’s more, both hormones irritate nerves and cause pain signals to be sent to the brain. This has a protective function: If the inflammation hurts, you tend to protect the affected part of the body and the pain stops you from using an injured joint.
- The inflammatory mediators have yet another function: They make it easier for immune system cells to pass out of the small blood vessels so that more of them can enter the affected tissue. The immune system cells also cause more fluid to enter the inflamed tissue, which is why it often swells.
- Mucous membranes also release more fluid when they are inflamed. For instance, this happens when you have a stuffy nose and the membranes lining your nose are inflamed. Then the extra fluid can help to quickly flush the viruses out of your body.2
 Understanding Chronic Inflammation.
Understanding Chronic Inflammation.
Signs of inflammation are like a car’s dashboard engine light. It tells you that something is wrong. Our response is not to take out the bulb, because that’s not the problem. Instead, we look at what caused the light to turn on. It’s the same with inflammation. It’s telling us that something bigger is going on that requires attention. When we take a drug to cover up the pain of inflammation it’s just like taking out the globe and expecting the problem to be resolved. It’s a bandaid approach rather than addressing the cause.
Risk Factors Associated with Chronic Inflammation.
Over half of us are living with chronic inflammation driven by diet, stress, and lack of sleep. Several risk factors promote a low-level inflammatory response.3 These include:
- Age: Increasing age is positively correlated with elevated levels of several inflammatory molecules. The age-associated increase in inflammatory molecules may be due to mitochondrial dysfunction or free radical accumulation over time and other age-related factors like an increase in visceral body fat.
- Obesity: Many studies have reported that fat tissue is an endocrine organ, secreting multiple adipokines and other inflammatory mediators. Some reports show that the body mass index of an individual is proportional to the amount of pro-inflammatory cytokines secreted. Metabolic syndrome typifies this well.
- Diet: A diet rich in saturated fat, trans-fats, or refined sugar is associated with higher production of pro-inflammatory molecules, especially in individuals with diabetes or overweight individuals.
 A diet rich in these foods is shown to increase inflammatory mediators:
A diet rich in these foods is shown to increase inflammatory mediators:
-
- Refined carbs
- Sugar
- Processed foods
- Fast food
- Industrial seed oils
- Fried food and rancid fats
- CAFO (concentrated animal feeding operation) animal proteins and dairy (high in omega-6 fats, which in excess can be inflammatory)
- Low Sex Hormones: Studies show that sex hormones like testosterone and estrogen can suppress the production and secretion of several pro-inflammatory markers and it has been observed that maintaining sex hormone levels reduces the risk of several inflammatory diseases.
- Stress and Sleep Disorders: Both physical and emotional stress is associated with inflammatory cytokine release. Stress can also cause sleep disorders. Since individuals with irregular sleep schedules are more likely to have chronic inflammation than consistent sleepers, sleep disorders are also considered as one of the independent risk factors for chronic inflammation. This makes stress a double whammy for immunity.
- Smoking: Cigarette smoking lowers the production of anti-inflammatory molecules and instigates inflammation of the arteries and other systems in the body.
Be sure to see our follow up blog How to Reduce the Chronic Inflammation in your Body.
Chronic Inflammation Can Result from the following:
These examples are in no order of their likelihood or importance.
- Failure of eliminating the agent causing acute inflammation, such as infectious organisms including Mycobacterium tuberculosis, protozoa, fungi, and other parasites that can resist host defenses and remain in the tissue for an extended period. Additionally, the failure or inability to eliminate heavy metals.
- Recurrent episodes of acute inflammation. However, in some cases, chronic inflammation is an independent response and not a sequel to acute inflammation, for example, diseases such as tuberculosis and rheumatoid arthritis. In rheumatoid arthritis, your immune system attacks your joints. You may experience joint pain, swelling, stiffness, or loss of joint function, fatigue, numbness and tingling, and limited range of motion.
- Liver dysfunction, resulting in an inability to clear pathogens and toxins from your body.
- Long term exposure to an irritant or foreign material, including substances or industrial chemicals that can be inhaled over a long period, for example, silica dust. Chemicals like this often cannot be eliminated by enzymatic breakdown or phagocytosis in the body.
This can also apply to the gut. Many people may not realise that simple chronic symptoms like bloating are a key factor in dysbiosis (or a gut imbalance favouring “bad” bugs over “good” ones), and what happens in the gut affects the entire body and even your brain.4
Take leaky gut, which is the link between gut health and systemic illness. “Leaky gut” is not a diagnosis but a process, a description of the underlying pathology of numerous diseases that we treat yet have failed to find a cure for. It is a condition in which connections between the cells that line the inside of the intestines (known as tight junctions) become looser, allowing larger molecules (such as partially digested food particles) to pass through the gut wall. Your immune system is constantly patrolling the gut border for anything it does not recognize in order to prevent an all-out invasion. As the immune system encounters these escaped particles, it attacks. In individuals with a genetic predisposition to autoimmune diseases, this increased load on the immune system leads to the type of dysregulation that becomes an autoimmune disease.
- With MTHFR mutations.
What is MTHFR? MTHFR is a genetic mutation that at least 40% of the population has. MTHFR or Methylenetetrahydrofolate Reductase is an enzyme that converts folic acid into methyl-folate (5MTHFR). Methyl-folate is the primary form of folate in our blood and is an important part of the body’s detoxification process doing so through a process called Methylation. MTHFR gene mutations create blockages that don’t allow all the body’s toxins to become detoxified due to being slowed by unmetabolized folic acid. Since our bodies have a hard time converting folic acid to methyl-folate, the unmetabolized folic acid sits in our bodies and so do the toxins. Without proper detoxification, our bodies tend to react to toxins in a negative way.
MTHFR mutations, therefore, are the root cause of inflammatory diseases. Remember one of the most important jobs that methylation does is flagging toxins for the liver to prepare for removal from the body. When the body starts detoxifying, the liver looks for these flagged toxins and metabolizes them for elimination.
The methylation deficiency caused by these mutations prevent toxins from being removed efficiently, therefore the accumulated built-up toxins result in inflammation.
What Can You Do? Remove toxins from the body. A toxic body results in inflammation, this chronic inflammation turns into inflammatory diseases and autoimmune reactions. Reducing inflammation and detoxification can lessen symptoms of autoimmune diseases while also supporting the immune system and enabling vitamins, antioxidants, and trace metals to work more effectively within the body.
- An Autoimmune disorder, in which the immune system recognises the normal component of the body as a foreign antigen, and attacks healthy tissue giving rise to diseases such as rheumatoid arthritis (RA), systemic lupus erythematosus (SLE). In some autoimmune conditions, your immune system affects your skin, leading to rashes. In other types, it attacks specific glands, which affect hormone levels in the body. Inflammatory bowel disease (IBD) represents a group of intestinal disorders that cause prolonged inflammation of the digestive tract. Many diseases are included in this IBD umbrella term. The two most common diseases are ulcerative colitis and Chron’s disease. IBD can also occur when the inflammation doesn’t go away after the infection is cured. The inflammation may continue for months or even years.
- Certain mediations
- Inflammatory and biochemical inducers that cause oxidative stress and mitochondrial dysfunction such as increased production of free radical molecules, advanced glycation end products (AGEs), uric acid (urate) crystals, and oxidized lipoproteins. Inflammation and oxidative stress are two sides of the same coin. When oxidation increases in your body, it causes more inflammation, and when inflammation increases, it causes more oxidative stress. For more information on this process please read our oxidative stress blog here…
- A defect in the cells responsible for mediating inflammation, leading to persistent or recurrent inflammation, such as auto-inflammatory disorders (Familial Mediterranean Fever). Yep, I’d not heard of this either!
Conditions Associated with Chronic Inflammation
Chronic inflammatory diseases represent the leading cause of death worldwide. While many diseases have inflammation as a contributing factor, below are the most prevalent conditions associated with chronic inflammation:

- Anxiety and depression
- Skin conditions like acne, eczema, and psoriasis
- Allergies
- Food and chemical sensitivities
- Asthma
- Chronic obstructive pulmonary disease (COPD)
- Immune challenges
- Diabetes
- High blood pressure, heart disease, and stroke
- Arthritis
- Autoimmune Conditions
- Ulcerative colitis
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Multiple sclerosis
- Alzheimer’s and other forms of dementia
- Cancer
Complications
Although chronic inflammation progresses silently, it is the cause of most chronic diseases and presents a major threat to the health and longevity of individuals. Inflammation is considered a major contributor to several diseases including3:
- Cardiovascular diseases: Many clinical studies have shown strong and consistent relationships between markers of inflammation such as hsCRP and cardiovascular disease. Furthermore, atherosclerosis is a pro-inflammatory state with all the features of chronic low-grade inflammation and leads to increase cardiovascular events such as myocardial infarction, stroke, among others.
- Cancer: Chronic low-level inflammation also appears to participate in many types of cancer such as kidney, prostate, ovarian, hepatocellular, pancreatic, colorectal, lung, and mesothelioma.
- Diabetes: Immune cells like macrophages infiltrate pancreatic tissues releasing pro-inflammatory molecules in diabetic individuals. Both circulating and cellular biomarkers underscore that diabetes is a chronic inflammatory disease. Chronic complications linked to diabetes include both microvascular and macrovascular complications. Diabetes not only increases the risk of macrovascular complications like strokes and heart attacks but also microvascular complications like diabetic retinopathy, neuropathy, and nephropathy.
- Rheumatoid arthritis: In a genetically susceptible host, chronic inflammation induced by several environmental factors such as smoking and infections lead to a systemic autoimmune response that causes a local inflammatory response in joints, infiltration of immune cells, and release of cytokines. The persistence of chronic inflammation in the synovium in inadequately treated RA has been associated with worse prognosis and radiographic progression of the disease.
- Allergic asthma: A complex, chronic inflammatory disorder associated with inappropriate immune response and inflammation in conducting airways involving a decline in airway function and tissue remodeling.
- Chronic obstructive pulmonary disease (COPD): An obstructive lung disease, develops as a chronic inflammatory response to inspired irritants and characterized by long-term breathing problems.
- Alzheimer’s disease: In older adults, chronic low-level inflammation is linked to cognitive decline and dementia.
- Chronic kidney disease (CKD): Low-grade inflammation is a common feature of chronic kidney It can lead to the retention of several pro-inflammatory molecules in the blood and contributes to the progression of CKD and mortality. Amyloidosis can be a result of underlying chronic inflammation that can lead to severe renal complications.
- Inflammatory Bowel Disease (IBD): is a group of chronic inflammatory disorders of the digestive tract. It can develop as ulcerative colitis causing long-lasting inflammation and ulcers in the lining of the large intestine and rectum or Crohn’s disease characterized by inflammation of the lining of the digestive tract dispersing into affected tissues such as the mouth, oesophagus, stomach, and the anus.
- Mood disorder. Researchers have found an association between fatigue, pain, and depressive symptoms. “Inflammation could be a common link between fatigue, pain, and depression,” researchers in one study concluded. As it turns out, a lot of these mood disorders are linked to poor gut health.5
 How is Inflammation Diagnosed?
How is Inflammation Diagnosed?
There’s no single test that can diagnose inflammation or conditions that cause it. Instead, based on your symptoms, your doctor may give you any of the tests below to make a diagnosis. There are a few so-called markers that help diagnose inflammation in the body. However, these markers are nonspecific, meaning that abnormal levels can show that something is wrong, but not what is wrong.
Blood Tests:
Serum protein electrophoresis (SPE) is considered to confirm chronic inflammation. It measures certain proteins in the liquid part of the blood to identify any issues. Too much or too little of these proteins can point to inflammation and markers for other conditions.
C-reactive protein (CRP): is naturally produced in the liver in response to inflammation. A high level of CRP in your blood can occur due to several inflammatory conditions. While this test is very sensitive for inflammation, it doesn’t help differentiate between acute and chronic inflammation, since CRP will be elevated during both. A CRP level between 1 and 3 milligrams per liter of blood often signals a low, yet chronic, level of inflammation. High levels combined with certain symptoms can help your doctor make a diagnosis.
Erythrocyte sedimentation rate (ESR):The ESR test is sometimes called a sedimentation rate test. This test indirectly measures inflammation by measuring the rate at which red blood cells sink in a tube of blood. The quicker they sink, the more likely you’re experiencing inflammation. The ESR test is rarely performed alone, as it doesn’t help pinpoint specific causes of inflammation. Instead, it can help your doctor identify that inflammation is occurring. It can also help them monitor your condition.
Plasma viscosity: This test measures the thickness of blood. Inflammation or infection can thicken plasma.
Other blood tests: If your doctor believes the inflammation is due to viruses or bacteria, they may perform other specific tests. In this case, your doctor can discuss what to expect with you.
Other Diagnostic Tests: If you have certain symptoms — for instance, chronic diarrhea or numbness on one side of your face — your doctor may request an imaging test to check certain parts of the body or brain. MRIs and X-rays are commonly used. To diagnose inflammatory gastrointestinal conditions, your doctor may perform a procedure to see inside parts of the digestive tract. These tests can include colonoscopy, sigmoidoscopy, upper endoscopy.
Be sure to see our follow up blog How to Reduce the Chronic Inflammation in your Body.
In health,
Dr. Jennifer Barham-Floreani,
Bach. Chiropractic, Bach. App Clinical Science
Registered internationally, no longer practicing as a chiropractor in Australia.
Wilem Floreani,
Research Assistant & Student
Barcelona College of Chiropractic
References:
- Chen L, Deng H, Cui H, et al. Inflammatory responses, and inflammation-associated diseases in organs. Oncotarget. 2017;9(6):7204-7218. Published 2017 Dec 14. doi:10.18632/oncotarget.23208
- org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. What is an inflammation? 2010 Nov 23 [Updated 2018 Feb 22]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279298/
- Pahwa R, Goyal A, Bansal P, et al. Chronic Inflammation. [Updated 2020 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://ncbi.nlm.nih.gov/books/NBK493173/
- Rowin J, Xia Y, Jung B, Sun J. Gut inflammation and dysbiosis in human motor neuron disease. Physiol Rep. 2017 Sep;5(18):e13443. do: 10.14814/phy2.13443. PMID: 28947596; PMCID: PMC5617930. Rowin J, Xia Y, Jung B, Sun J. Gut inflammation and dysbiosis in human motor neuron disease. Physiol Rep. 2017 Sep;5(18):e13443. do: 10.14814/phy2.13443. PMID: 28947596; PMCID: PMC5617930.
- Louati K, Berenbaum F. Fatigue in chronic inflammation – a link to pain pathways. Arthritis Res Ther. 2015;17:254. Published 2015 Oct 5. doi:10.1186/s13075-015-0784-1